Andrigolitis is an emerging health condition that is believed to involve ongoing inflammation of body tissues. Though the name may sound unfamiliar to many, conditions involving chronic inflammation are not new in the medical world.
Andrigolitis is thought to affect different parts of the body, including joints, muscles, and possibly internal organs, leading to discomfort, reduced mobility, and tiredness.
As research is still in its early stages, information about the disease is growing slowly. People are increasingly curious to understand what triggers Andrigolitis, how it can be detected early, and whether it can be managed or cured.
Understanding such conditions early can make a huge difference in treatment success. Learning about Andrigolitis is important not only for those who might suffer from it but also for families, friends, and healthcare workers who support them.
Knowledge is the first step toward empowerment, and by the end of this article, you will be more prepared to recognize, manage, and support people dealing with Andrigolitis.
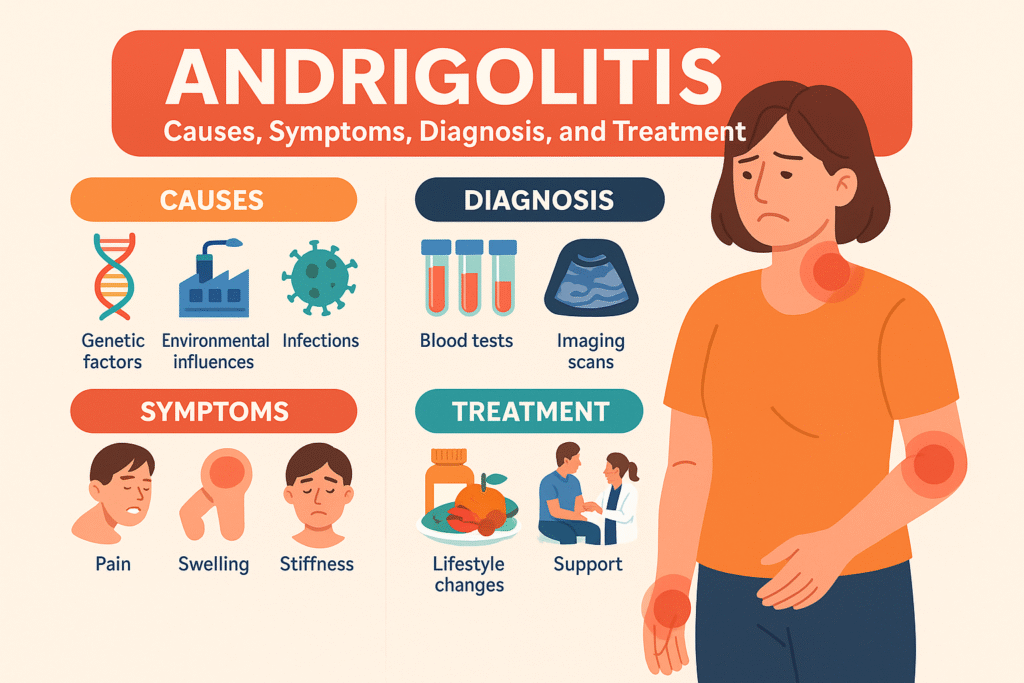
Possible Causes of Andrigolitis
Scientists and doctors are exploring the various causes of Andrigolitis, but no single cause has been confirmed yet. Instead, it appears to be the result of multiple overlapping factors.
One important area being studied is genetics. Some families may pass down genes that make people more prone to inflammatory conditions. If a close family member has autoimmune diseases or arthritis, the risk might be higher.
Environmental factors are another strong suspect. Continuous exposure to polluted air, harmful chemicals, or allergens might trigger unwanted inflammation inside the body. Living in highly polluted cities or working with chemicals without protection could potentially increase the risk.
Lifestyle choices are also believed to play a major role. Poor diet, smoking, lack of exercise, chronic stress, and poor sleep habits all weaken the immune system and open the door to long-term health issues like Andrigolitis.
Another interesting factor being investigated is the impact of infections. Sometimes a viral or bacterial infection confuses the immune system, causing it to attack healthy tissues mistakenly even after the infection clears.
Overall, Andrigolitis is likely caused by a combination of genetic weakness, environmental exposure, infections, and unhealthy living habits — not just one thing alone.
Signs and Symptoms of Andrigolitis
Because Andrigolitis is related to inflammation, many of its symptoms are connected to swelling, pain, and discomfort. However, the symptoms can vary a lot depending on which body parts are affected.
Common symptoms include:
- Persistent pain in joints, muscles, or other tissues even without any clear injury.
- Swelling and redness around affected areas.
- Stiffness, especially in the morning or after long periods of rest.
- Extreme tiredness or fatigue that does not go away even after sleep.
- Mild fevers or flu-like symptoms from the body fighting inflammation.
- Appetite loss and unintended weight changes.
- Mood changes like sadness or irritability, which often come from constant discomfort.
In some rare cases, if Andrigolitis affects internal organs like the heart or lungs, it can cause chest pain, shortness of breath, or digestive problems.
It is very important to recognize these symptoms early. Ignoring them can cause the condition to worsen, leading to permanent damage in joints, muscles, or organs.
How Andrigolitis Might Be Diagnosed
Diagnosing Andrigolitis is often challenging, especially because it shares many symptoms with better-known diseases like rheumatoid arthritis, lupus, or fibromyalgia.
Doctors usually follow a careful step-by-step method to make sure the diagnosis is correct.
First, a detailed patient history is taken, covering symptoms, lifestyle, and family health background. Next, a physical examination is done to check for swelling, tenderness, movement difficulty, or skin changes.
Several medical tests might be ordered:
- Blood tests to check inflammation markers like ESR (erythrocyte sedimentation rate) or CRP (C-reactive protein).
- Autoimmune tests to rule out diseases like lupus.
- Imaging scans like X-rays, MRI, or ultrasound to look for hidden joint or tissue damage.
- Biopsies (small tissue samples) in rare cases, if internal organs are suspected to be affected.
Because no single test confirms Andrigolitis, diagnosis often depends on combining all these clues. Getting a second opinion from a specialist, like a rheumatologist, is sometimes advised.
Treatment Options for Andrigolitis
There is no universal cure for Andrigolitis yet, but treatments aim to control inflammation, reduce pain, and improve quality of life.
Here are the main treatment approaches:
- Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen help with pain and swelling. In moderate cases, doctors might prescribe corticosteroids to quickly calm down inflammation.
- Immune-modulating drugs: In more serious cases, medicines that adjust how the immune system works may be used to prevent it from attacking the body.
- Physical therapy: Exercises and movement therapies keep joints flexible and muscles strong. Physical therapy reduces stiffness and prevents deformities.
- Lifestyle changes: Eating an anti-inflammatory diet (rich in fruits, vegetables, and healthy fats), avoiding junk food, quitting smoking, and reducing alcohol intake are crucial.
- Mental health support: Chronic illnesses often cause emotional strain. Counseling or therapy helps manage stress, anxiety, or depression.
Surgery is very rare and is usually only considered if there is severe joint or tissue damage that doesn’t respond to other treatments.
Managing Andrigolitis Daily
Managing Andrigolitis every day requires patience, discipline, and positivity. Small daily habits can make a big difference over time.
Key management strategies include:
- Balanced Diet: Omega-3 fatty acids (found in fish like salmon), berries, leafy greens, and nuts help naturally fight inflammation. Avoid processed foods, sugars, and fried items.
- Gentle Exercise: Activities like swimming, cycling, tai chi, and yoga keep the body active without stressing the joints. Even simple stretching every morning can help maintain flexibility.
- Good Sleep Habits: Creating a relaxing bedtime routine ensures the body has time to repair itself.
- Flare-up Planning: Having a plan (like resting, applying ice/heat packs, or adjusting medicines) when symptoms flare up can prevent panic and worsening.
- Social Support: Joining patient support groups, whether online or offline, reduces loneliness and provides emotional encouragement.
A person with Andrigolitis needs to listen to their body daily — knowing when to push and when to rest is crucial for living well.
Preventive Measures Against Andrigolitis
Although not every case of Andrigolitis can be prevented, healthy living drastically reduces the risk or severity.
Important preventive tips:
- Maintain a healthy weight to reduce pressure on joints.
- Exercise regularly to strengthen the body’s natural defenses.
- Eat smart with anti-inflammatory foods and limit harmful processed foods.
- Manage mental health through mindfulness, meditation, or therapy.
- Get regular medical checkups, especially if you have a family history of inflammatory or autoimmune diseases.
By adopting these habits early, even people at higher genetic risk can potentially delay or lessen the impact of Andrigolitis.
Living with Andrigolitis: Real-Life Perspective
Many people who have Andrigolitis show incredible strength by adjusting their lifestyles and continuing to chase their dreams.
They accept the need for change but do not let the illness define them.
Small changes like using ergonomic furniture, adjusting work hours, or planning restful weekends allow patients to stay productive.
Many also discover new passions — painting, writing, mentoring others — that fit their new pace of life.
The emotional journey is not easy. Some days are frustrating, but a strong support network and mental resilience help overcome challenges.
Sharing real stories builds hope for newcomers who may feel scared when first diagnosed.
Research and Future Directions
Medical science is making exciting progress in understanding inflammatory diseases like Andrigolitis.
Researchers are investigating biologic therapies that target very specific parts of the immune system rather than using general drugs.
Gene therapy, stem cell research, and precision medicine (treatments tailored to an individual’s DNA) are some futuristic methods being tested.
Tech tools like health monitoring apps, wearable devices, and online consultation services are already making life easier for many patients.
There is hope that within the next decade, Andrigolitis will become much easier to diagnose, treat, and maybe even cure.
The growing awareness about invisible illnesses is also improving workplace laws, insurance coverage, and public understanding, giving more dignity and support to those living with chronic conditions.
Conclusion
Andrigolitis might be a new name in the medical world, but its challenges are real and deserve attention.
Through early recognition, proper diagnosis, personalized treatment, and healthy daily living, people affected by Andrigolitis can still lead meaningful, active, and happy lives.
Ongoing research, patient resilience, and global awareness offer a brighter future.
Whether you are a patient, a friend, or a healthcare provider, staying informed about Andrigolitis empowers you to act with confidence and compassion.
Remember, the journey with Andrigolitis is not one of defeat — it is a journey of adaptation, strength, and hope.
FAQs
What is Andrigolitis and who can get it?
Andrigolitis is a newly recognized inflammatory condition that can affect people of any age, but may be more common in adults with genetic risk factors.
What are the first warning signs of Andrigolitis?
Early signs often include unexplained joint pain, fatigue, stiffness, and swelling that doesn’t improve with rest.
Can Andrigolitis be cured completely?
There is no permanent cure yet, but early diagnosis and proper treatment can control symptoms and improve quality of life.
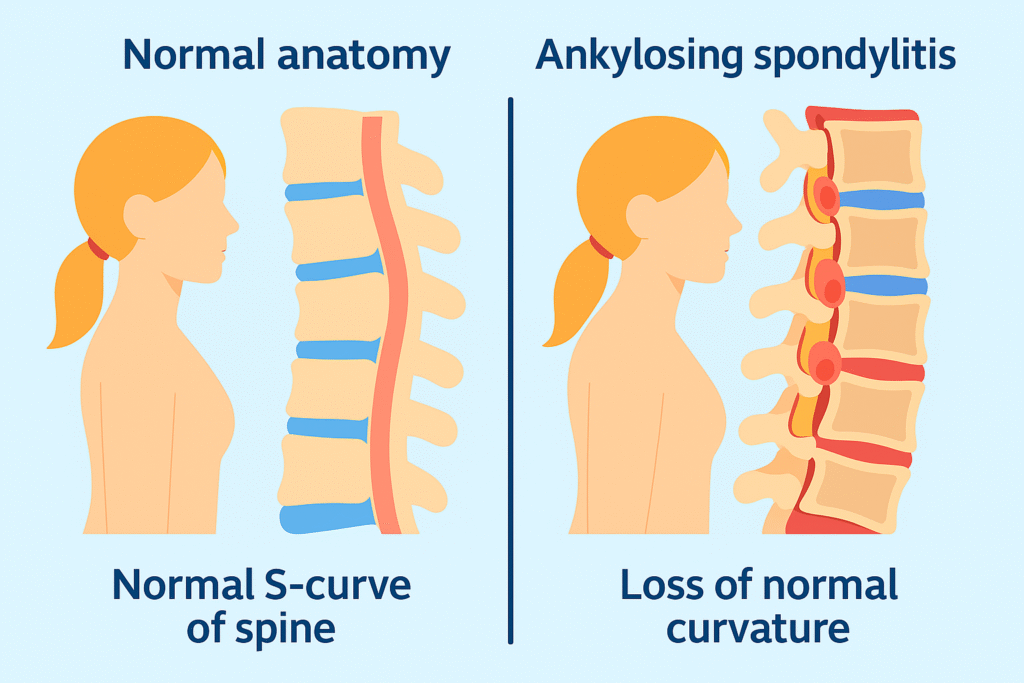
How is Andrigolitis different from arthritis?
While both involve inflammation, Andrigolitis may affect multiple tissues, not just joints, and has a broader set of symptoms.
What lifestyle changes help manage Andrigolitis better?
Eating an anti-inflammatory diet, exercising gently, managing stress, and following medical advice can greatly reduce flare-ups.
Also Read:
Directory ArcyArt: Why It’s a Game-Changer for Independent Artists
Immediate 0.3 Folex: How This AI Platform Changes Crypto and Forex Trading
letsbuildup org: Why It Matters for Personal Growth and Environmental Health
odysseystoryshop.com: Why Personalized Gifts Are the New Trend